Edema Nursing Diagnosis: From Symptoms to Successful Care
Edema, characterized by the swelling of body tissues due to excess fluid accumulation, is a common clinical finding. While often a symptom of an underlying condition, it can significantly impact a patient’s comfort and well-being. As a nurse, understanding the nuances of edema, from its presentation to its management, is critical for providing effective patient care. This article provides a comprehensive overview of the edema nursing diagnosis, covering its symptoms, diagnostic approaches, nursing interventions, and strategies for successful patient care.
Understanding Edema: What Nurses Need to Know
Edema is not a disease itself but rather a symptom of an underlying medical issue. Fluid leaks from the blood vessels into the surrounding tissues, leading to swelling. The location and severity of edema can vary widely, impacting different body systems.
Key Considerations for Nurses:
- Types of Edema:
- Peripheral Edema: Affects the extremities (legs, feet, ankles, hands).
- Pulmonary Edema: Fluid accumulation in the lungs, a life-threatening condition.
- Cerebral Edema: Swelling of the brain.
- Ascites: Fluid accumulation in the abdominal cavity.
- Causes of Edema: Can stem from various factors, including:
- Cardiac Issues: Heart failure, valve disorders.
- Renal Issues: Kidney disease, nephrotic syndrome.
- Hepatic Issues: Liver cirrhosis.
- Venous Insufficiency: Varicose veins, deep vein thrombosis (DVT).
- Lymphatic Obstruction: Lymphedema.
- Medications: Certain drugs can cause fluid retention (e.g., NSAIDs, corticosteroids).
- Nutritional Deficiencies: Malnutrition, protein deficiency.
- Pregnancy: Physiological edema.
- Importance of Accurate Assessment: A thorough assessment is crucial to identify the cause of edema, guide treatment, and monitor the patient’s response to interventions.
Identifying Edema: Recognizing the Symptoms
The presentation of edema can vary depending on its location and severity. As a nurse, you’ll be the first point of contact to identify and assess.
Common Signs and Symptoms:
- Visible Swelling: The most obvious sign, often appearing in the extremities.
- Pitting Edema: Indentation remains after pressing the swollen area. (Graded on a scale from 1+ to 4+ based on depth and duration of indentation).
- Skin Changes: Stretched or shiny skin, warmth, redness, or changes in skin texture.
- Increased Abdominal Girth: In cases of ascites.
- Shortness of Breath: In pulmonary edema.
- Coughing or Wheezing: In pulmonary edema.
- Weight Gain: Often a significant indicator of fluid retention.
- Reduced Urine Output: The kidneys may be retaining fluid.
- Pain or Discomfort: Depending on the cause and location.
Nursing Diagnosis and Assessment: Pinpointing the Problem
A successful nursing diagnosis for edema relies on a comprehensive assessment. This involves gathering subjective and objective data to determine the underlying cause and develop an effective care plan.
Key Assessment Components:
- Patient History:
- Medical History: Identify any pre-existing conditions that could contribute to edema (e.g., heart failure, kidney disease).
- Medication History: Review all medications, including over-the-counter drugs and herbal supplements.
- Dietary Habits: Assess sodium and fluid intake.
- Symptoms and Onset: Determine the location, duration, and characteristics of the edema.
- Physical Examination:
- Vital Signs: Monitor blood pressure, heart rate, respiratory rate, and oxygen saturation.
- Edema Assessment: Inspect and palpate for swelling, pitting, and skin changes. Measure limb circumference.
- Auscultation: Listen to lung sounds for crackles or wheezes (pulmonary edema). Listen to heart sounds for murmurs or gallops.
- Abdominal Examination: Assess for distension, tenderness, and ascites.
- Diagnostic Tests:
- Blood Tests: Complete blood count (CBC), electrolytes, kidney function tests (BUN, creatinine), liver function tests (LFTs), albumin levels.
- Urine Tests: Urinalysis to assess kidney function.
- Imaging Studies: Chest X-ray (pulmonary edema), echocardiogram (heart function), ultrasound (assess for DVT or ascites).
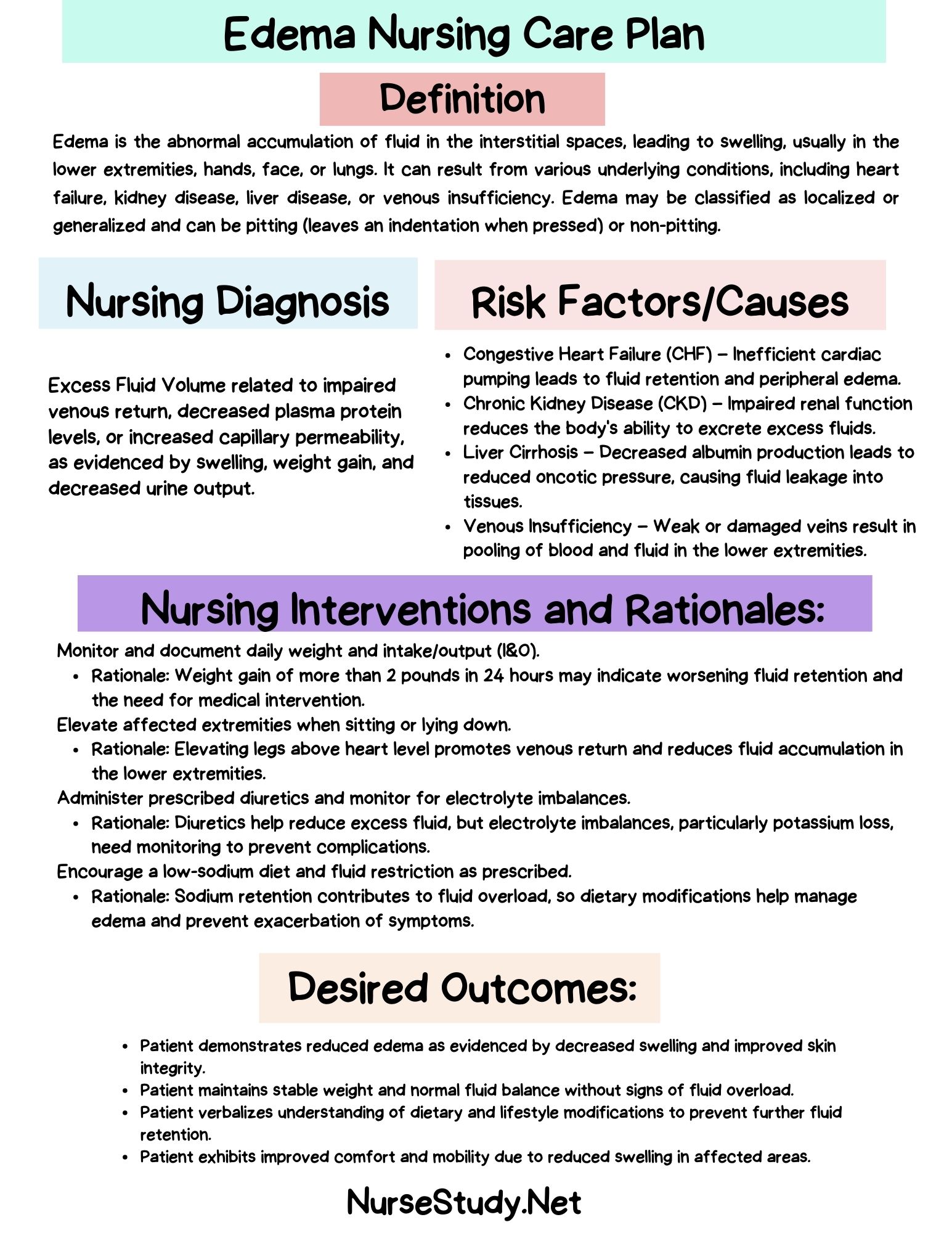
Common Nursing Diagnoses Related to Edema:
- Excess Fluid Volume
- Impaired Gas Exchange (in pulmonary edema)
- Decreased Cardiac Output (related to underlying cardiac issues)
- Activity Intolerance
- Impaired Skin Integrity (related to edema and skin changes)
- Risk for Impaired Tissue Perfusion (related to edema and vascular issues)
Nursing Interventions for Edema Management
The primary goal of nursing interventions is to address the underlying cause of edema, reduce fluid accumulation, and improve patient comfort.
Key Nursing Interventions:
- Fluid Management:
- Fluid Restriction: As prescribed by the physician, especially for patients with heart failure or kidney disease.
- Accurate Intake and Output (I&O) Monitoring: Track fluid intake (oral, intravenous) and output (urine, drains).
- Daily Weights: Monitor weight changes, a crucial indicator of fluid retention.
- Medication Administration:
- Diuretics: Administer prescribed diuretics (e.g., furosemide, bumetanide, spironolactone) to promote fluid excretion.
- Monitor Electrolyte Levels: Be vigilant for electrolyte imbalances (e.g., hypokalemia, hyponatremia) associated with diuretic use.
- Medication Education: Educate the patient on the purpose, dosage, side effects, and administration of medications.
- Positioning and Comfort:
- Elevate Edematous Extremities: Elevate legs and feet to promote venous return and reduce swelling.
- Reposition Patient Regularly: Prevent skin breakdown, especially in areas with edema.
- Provide Skin Care: Keep skin clean and dry, apply lotion to moisturize and prevent breakdown.
- Pressure Relief: Use pressure-relieving devices (e.g., pillows, foam pads) to protect edematous areas.
- Nutrition:
- Sodium Restriction: Educate the patient on a low-sodium diet (avoiding processed foods, canned goods, and salty snacks).
- Monitor Nutritional Status: Assess for signs of malnutrition (which can worsen edema).
- Monitoring and Evaluation:
- Monitor Vital Signs: Track blood pressure, heart rate, respiratory rate, and oxygen saturation.
- Assess Edema: Regularly assess the location, severity, and pitting characteristics of edema.
- Monitor Respiratory Status: Watch for signs of pulmonary edema (shortness of breath, cough, wheezing).
- Evaluate Response to Interventions: Assess the effectiveness of nursing interventions and adjust the care plan as needed.
Promoting Patient Education and Discharge Planning
Patient education is crucial for long-term management and preventing complications.
Key Areas for Patient Education:
- Understanding Edema: Explain the cause of edema and its relationship to their medical condition.
- Medication Management: Emphasize the importance of taking medications as prescribed and reporting any side effects.
- Dietary Modifications: Provide guidance on sodium restriction and healthy eating habits.
- Fluid Management: Explain fluid restrictions, if applicable, and how to monitor fluid intake.
- Activity and Exercise: Encourage moderate activity and exercise, as tolerated, to promote circulation.
- Skin Care: Teach patients how to care for their skin to prevent breakdown and infection.
- Signs and Symptoms to Report: Instruct patients to report any worsening of symptoms (e.g., increased swelling, shortness of breath, chest pain) immediately.
Discharge Planning:
- Medication Reconciliation: Ensure a complete list of medications is provided to the patient and any new medications.
- Home Health Referrals: Consider home health care for patients needing assistance with medication management, wound care, or other needs.
- Follow-Up Appointments: Schedule follow-up appointments with the physician and other healthcare providers.
Conclusion: Providing Compassionate and Effective Care
Edema management requires a comprehensive approach, from meticulous assessment and accurate diagnosis to implementing appropriate nursing interventions and providing patient education. By understanding the underlying causes of edema, recognizing its signs and symptoms, and implementing evidence-based nursing practices, nurses can significantly improve patient outcomes and enhance their quality of life. The key is to provide compassionate, individualized care that addresses the patient’s physical and emotional needs.
FAQs about Edema Nursing Diagnosis
1. What is the difference between pitting and non-pitting edema?
Pitting edema leaves an indentation when pressure is applied, indicating fluid accumulation in the interstitial space. Non-pitting edema does not leave an indentation, suggesting other factors are involved, such as lymphatic obstruction or inflammation.
2. What are the potential complications of untreated edema?
Untreated edema can lead to various complications, including impaired wound healing, skin breakdown, increased risk of infection, difficulty breathing (in pulmonary edema), and decreased mobility.
3. How can a nurse help a patient with edema at home?
Nurses can educate patients on home management strategies, including medication adherence, dietary restrictions, elevation of edematous limbs, skin care, and monitoring weight and symptoms. They can also arrange for home health visits if needed.
4. What is the role of compression stockings in edema management?
Compression stockings help to improve venous return and reduce swelling in the lower extremities. Nurses can educate patients on proper application, removal, and care of compression stockings, which can be a key part of a treatment plan.
5. When should a patient with edema seek immediate medical attention?
A patient with edema should seek immediate medical attention if they experience sudden onset of swelling, shortness of breath, chest pain, severe abdominal pain, or any other concerning symptoms.