Decoding the Sounds: Negative Bronchophony – Diagnosis, Treatment, and What You Need to Know
Are you experiencing persistent coughs, shortness of breath, or chest discomfort? Your doctor might conduct a physical examination, including auscultation – listening to your lungs with a stethoscope. One key aspect of this exam is assessing for bronchophony. While the term itself might sound intimidating, understanding it is crucial for comprehending your respiratory health. This article delves into negative bronchophony, its diagnosis, potential causes, treatment options, and what you need to know to navigate this medical territory.
What is Bronchophony? Understanding the Basics
Bronchophony is a specific sound heard during auscultation. It’s the enhanced transmission of vocal sounds through the lungs. Essentially, the doctor asks you to say “99” or “one-two-three” while listening with the stethoscope.
- Normal Lungs: In healthy lungs, the vocal sounds are muffled and indistinct.
- Positive Bronchophony: This indicates that the vocal sounds are clear, loud, and easily understood. This is often a sign of lung consolidation, where the air-filled lung tissue is replaced with fluid or solid material (e.g., pneumonia, lung abscess).
- Negative Bronchophony: This, conversely, means that the vocal sounds are less audible or absent altogether. This can also be a sign of underlying lung issues.
Unpacking Negative Bronchophony: What Does It Mean?
Negative bronchophony, while not as commonly discussed as its positive counterpart, can be a significant indicator of certain lung conditions. It suggests an obstruction or blockage preventing sound waves from reaching the stethoscope as clearly. This obstruction could be caused by a variety of factors.
Potential Causes of Negative Bronchophony
Several underlying conditions can lead to negative bronchophony. These include:
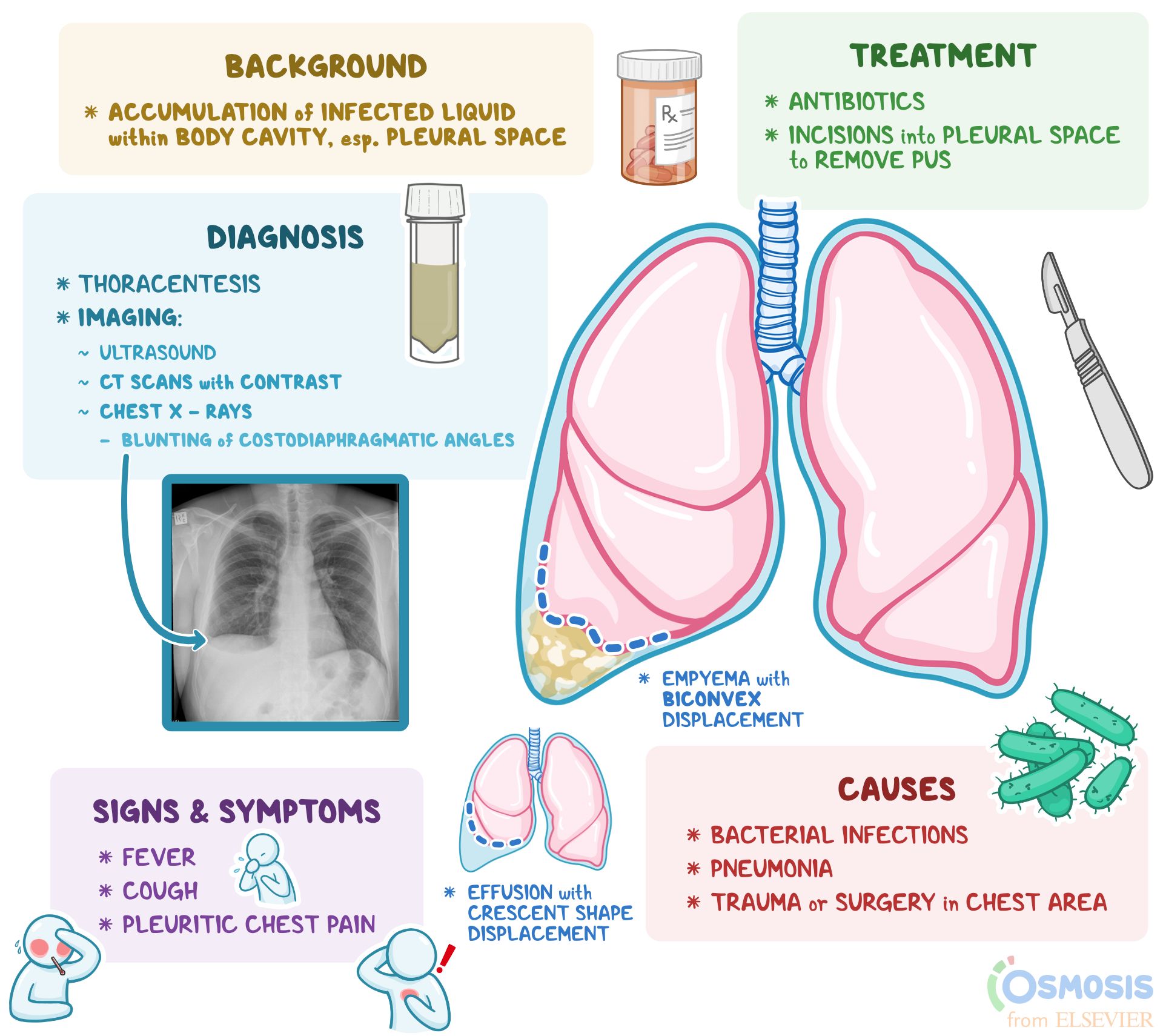
- Pleural Effusion: Fluid accumulation in the space between the lungs and the chest wall. The fluid acts as a barrier, dampening sound transmission.
- Pneumothorax: The presence of air in the pleural space, causing the lung to collapse. The air similarly interferes with sound conduction.
- Emphysema: A chronic lung disease that damages the air sacs (alveoli) in the lungs. This can make sound transmission less efficient.
- Lung Obstruction: Blockage of an airway, such as from a tumor, mucus plug, or foreign object.
- Severe Atelectasis: Collapse of a large portion of a lung.
Diagnosing Negative Bronchophony: A Comprehensive Approach
Diagnosing negative bronchophony involves a combination of assessments:
- Medical History and Physical Examination: The doctor will ask about your symptoms, medical history, and perform a physical examination, including auscultation.
- Imaging Tests:
- Chest X-ray: Can visualize fluid, air, or masses in the chest.
- CT Scan: Provides more detailed images of the lungs and surrounding structures.
- Pulmonary Function Tests (PFTs): Assess lung capacity and airflow.
- Other Tests: Depending on the suspected cause, other tests like blood tests, bronchoscopy (examining the airways with a scope), or thoracentesis (draining fluid from the pleural space) might be necessary.
Treatment Strategies for Conditions Associated with Negative Bronchophony
The treatment for negative bronchophony depends entirely on the underlying cause. The goal is to address the root problem and restore normal lung function. Here are some potential treatment approaches:
- Pleural Effusion: Treatment focuses on removing the fluid. This can involve:
- Thoracentesis: Draining the fluid with a needle.
- Drainage tubes: Inserting a tube to continuously drain fluid.
- Treating the underlying cause: Such as heart failure or infection.
- Pneumothorax: Treatment aims to remove the air and re-expand the lung:
- Observation: For small pneumothoraces, observation may be sufficient.
- Needle aspiration: Removing air with a needle.
- Chest tube insertion: Inserting a tube to continuously drain air.
- Emphysema: Management focuses on slowing the progression of the disease and managing symptoms:
- Smoking cessation: The most critical step.
- Medications: Bronchodilators, inhaled corticosteroids, and antibiotics for infections.
- Pulmonary rehabilitation: Exercises and education to improve lung function.
- Oxygen therapy: If oxygen levels are low.
- Lung Obstruction: Treatment depends on the cause of the obstruction:
- Removal of foreign object: If applicable.
- Medications: To reduce inflammation or open airways.
- Surgery: To remove tumors or other blockages.
- Severe Atelectasis: Treatment depends on the cause:
- Deep breathing exercises and coughing: To clear secretions.
- Bronchoscopy: To remove mucus plugs or other obstructions.
The Importance of Prompt Medical Attention
If you experience symptoms like shortness of breath, chest pain, persistent cough, or fever, and your doctor detects negative bronchophony, seeking prompt medical attention is crucial. Early diagnosis and treatment can significantly improve outcomes and prevent complications. Don’t delay seeking medical advice.
Frequently Asked Questions (FAQs)
1. What is the difference between bronchophony and egophony?
Both are vocal sounds assessed during auscultation. Bronchophony refers to the clarity of the spoken voice sounds, while egophony refers to the sound heard as “a-a-a” (like a bleating goat). Egophony often indicates consolidation or fluid in the lungs, similar to positive bronchophony.
2. Is negative bronchophony always a sign of a serious condition?
Not necessarily. While it can indicate serious conditions, it’s always assessed in conjunction with other symptoms and diagnostic tests. The underlying cause will determine the severity.
3. Can I diagnose negative bronchophony myself?
No. This is a clinical finding made by a trained medical professional using a stethoscope. Self-diagnosis is inaccurate and can lead to delayed treatment.
4. What if I’m diagnosed with a condition associated with negative bronchophony?
Follow your doctor’s treatment plan diligently. Attend all follow-up appointments, take medications as prescribed, and report any changes in your symptoms.
5. What lifestyle changes can help with conditions that can cause negative bronchophony?
Quitting smoking is paramount for conditions like emphysema. Avoiding irritants, practicing good hygiene to prevent infections, and maintaining a healthy weight are also important. Following a doctor’s advice is essential.
Conclusion: Taking Control of Your Respiratory Health
Negative bronchophony, while a specific medical term, is a valuable piece of the puzzle in understanding your lung health. By understanding its meaning, potential causes, and the diagnostic and treatment processes, you can become a more informed and proactive participant in your care. If you experience concerning respiratory symptoms, don’t hesitate to consult your doctor. Early intervention is key to managing these conditions and maintaining optimal lung function.