Navigating Polymicrogyria: Diagnosis, Life Expectancy, and Comprehensive Care
Polymicrogyria (PMG) is a complex neurological condition that presents a unique set of challenges for individuals and families. Characterized by an abnormally folded cerebral cortex, PMG can manifest in a wide range of severities, significantly impacting development and function. Understanding PMG, from its diagnosis to the ongoing care and support needed, is crucial for navigating the journey and providing the best possible quality of life. This comprehensive guide delves into the critical aspects of PMG, offering clarity and actionable information.
Understanding Polymicrogyria: What is It?
Polymicrogyria literally translates to “many small gyri” – referring to the brain’s outer layer (cortex). In individuals with PMG, the normally smooth surface of the cortex develops an unusually folded appearance. Instead of the typical large folds (gyri) and grooves (sulci), the brain exhibits numerous small, abnormally shaped folds. This disruption in brain structure can lead to a variety of neurological symptoms, the severity of which depends on the location and extent of the affected areas.
Diagnosing Polymicrogyria: The Path to Understanding
The diagnostic process for PMG typically involves a combination of methods, aiming to identify the characteristic brain malformation and rule out other potential causes of symptoms.
- Medical History and Physical Examination: The diagnostic journey often begins with a detailed review of the patient’s medical history, including developmental milestones, any observed symptoms, and family history of neurological conditions. A thorough physical and neurological examination helps assess motor skills, reflexes, and other neurological functions.
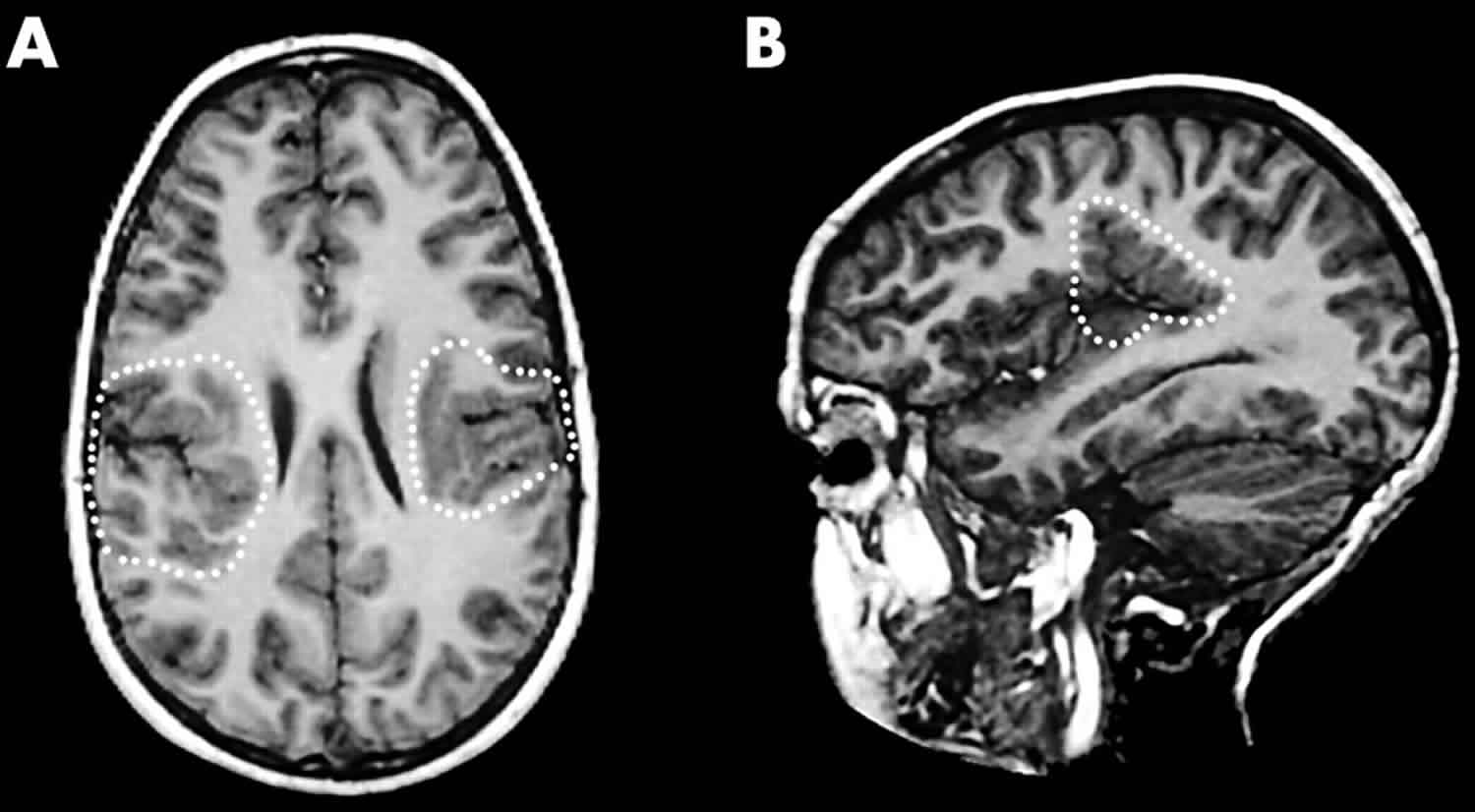
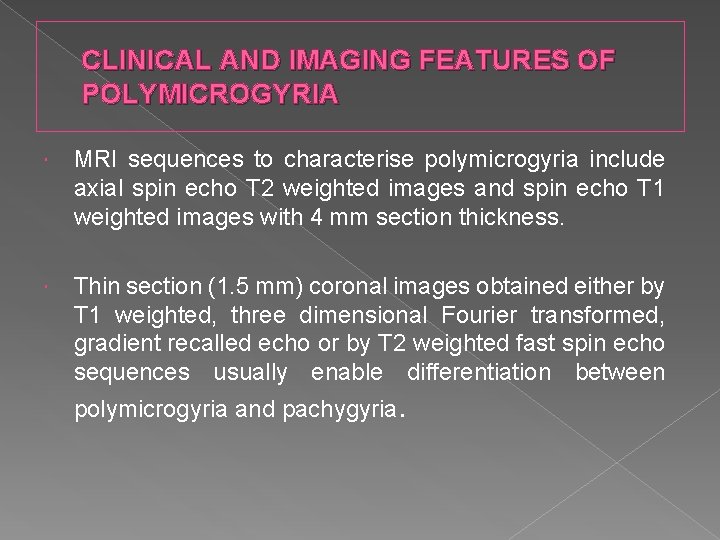
- Neuroimaging: This is a cornerstone of PMG diagnosis.
- Magnetic Resonance Imaging (MRI): MRI scans are particularly effective at visualizing the brain’s structure. They can reveal the characteristic small, irregular folds of the cortex associated with PMG. The MRI provides detailed images that help determine the extent and location of the malformation.
- Computed Tomography (CT) Scan: While not as detailed as an MRI, a CT scan can also be used to assess the brain and may detect some PMG-related changes, particularly in certain cases.
- Electroencephalogram (EEG): An EEG measures the electrical activity in the brain and can help identify seizure activity, a common symptom in individuals with PMG.
- Genetic Testing: Genetic testing may be recommended to identify underlying genetic causes of PMG. This can involve analyzing a panel of genes known to be associated with brain development. In some cases, whole-exome or whole-genome sequencing may be considered.
Life Expectancy and Polymicrogyria: What to Expect
Determining life expectancy in individuals with PMG is challenging due to the wide range of severity and the variability of symptoms. The prognosis is heavily influenced by several factors:
- Severity of Brain Malformation: The more extensive the PMG, the more severe the neurological impact, and potentially, the shorter the life expectancy.
- Presence and Control of Seizures: Uncontrolled seizures can significantly impact life expectancy. Effective management of seizures is crucial.
- Severity of Associated Conditions: PMG can be associated with other health complications, such as feeding difficulties, respiratory problems, and developmental delays, all of which can affect life expectancy.
- Access to Quality Care: Comprehensive medical care, including specialized therapies and support services, plays a vital role in managing symptoms and improving the quality of life and, potentially, life expectancy.
While some individuals with mild forms of PMG may live relatively long lives, others with more severe forms may face a shorter life expectancy. It’s crucial to consult with a neurologist and healthcare team to understand the specific prognosis for each individual case. Regular check-ups, early intervention, and comprehensive care are essential.
Comprehensive Care and Support for Individuals with PMG
Managing PMG requires a multidisciplinary approach, involving a team of healthcare professionals dedicated to providing comprehensive care.
- Neurologist: A neurologist specializes in diagnosing and treating neurological disorders and plays a central role in managing PMG.
- Pediatrician (for children): A pediatrician provides general medical care and coordinates other specialists’ care.
- Physical Therapist: Physical therapy helps improve motor skills, coordination, and mobility.
- Occupational Therapist: Occupational therapy focuses on improving daily living skills, such as feeding, dressing, and self-care.
- Speech Therapist: Speech therapy addresses communication difficulties, including speech delays, swallowing problems, and feeding issues.
- Developmental Pediatrician/Psychologist: These professionals can assess cognitive and developmental progress and provide behavioral support.
- Other Specialists: Depending on the specific symptoms, other specialists, such as a gastroenterologist (for feeding issues), pulmonologist (for respiratory problems), and ophthalmologist (for vision issues), may be involved.
Key aspects of care include:
- Seizure Management: Anti-seizure medications are often prescribed to control seizures. Regular monitoring and adjustments to medication are frequently necessary.
- Physical Therapy: Physical therapy helps improve motor skills, coordination, and mobility.
- Occupational Therapy: Occupational therapy focuses on improving daily living skills, such as feeding, dressing, and self-care.
- Speech Therapy: Speech therapy addresses communication difficulties, including speech delays, swallowing problems, and feeding issues.
- Assistive Devices: Depending on the individual’s needs, assistive devices, such as walkers, wheelchairs, and communication aids, may be beneficial.
- Nutritional Support: If there are feeding difficulties, nutritional support, which may include modified diets, feeding tubes, and specialized feeding techniques, may be necessary.
- Early Intervention Programs: Early intervention programs for infants and young children can provide crucial support for development and learning.
- Parent Support Groups: Connecting with other families facing similar challenges can provide emotional support, practical advice, and a sense of community.
Conclusion: Empowering Individuals with PMG
Living with polymicrogyria presents unique challenges, but with a proactive approach to diagnosis, care, and support, individuals and families can navigate this journey with resilience and hope. Understanding the nuances of PMG, from the diagnostic process to the importance of comprehensive care, is the first step toward improving the quality of life and maximizing potential. By working closely with a dedicated medical team and accessing available resources, individuals with PMG can thrive and live fulfilling lives.
Frequently Asked Questions (FAQs)
1. What causes Polymicrogyria?
The causes of PMG are diverse and can include genetic mutations, infections during pregnancy (such as cytomegalovirus or CMV), disruptions in blood supply to the developing brain, and exposure to certain substances during pregnancy. Sometimes, the cause remains unknown.
2. Can Polymicrogyria be cured?
Currently, there is no cure for PMG. However, the symptoms can be managed through various therapies and interventions. The focus of treatment is on managing symptoms, improving quality of life, and providing support to the individual and their family.
3. What are the common symptoms of Polymicrogyria?
Symptoms vary depending on the location and extent of the brain malformation. Common symptoms include developmental delays, intellectual disabilities, seizures, motor impairments (such as cerebral palsy), feeding difficulties, and speech and language problems.
4. How can I find support for my child or loved one with PMG?
Connect with your healthcare team for referrals to specialists and support services. Look for local and national support groups for families affected by neurological conditions. Online forums and communities can also provide valuable information and emotional support.
5. What is the role of genetic testing in PMG?
Genetic testing can help identify the underlying cause of PMG, which can inform prognosis and future family planning. It can also provide valuable information about the specific genetic mutations associated with the condition, which can help guide treatment and management.